In this month of re-commitment to fighting Breast cancer, it is imperative to stop a while in a moment of reflection for those who have lost the fight, remind ourselves of who they were, what lives they touched as they made us who we are today in many ways. I remember my mother who was afflicted by this disease, a kind loving soul, who despite our number (family of 15) had managed to make all of us feel special. I grew up truly believing that of all her kids, I was the one. But talking to my other siblings, each one of us felt that special feeling! In 1974, 3 years before she was diagnosed and treated in Belgium, she added to my name a secret portion, "Muendela yenda" (the one who will walk alone) and here I am today, far from the country of origin, in El Paso, Texas, the sole American Citizen of my family! Preaching to a silent choir on this blog. Breast cancer victims are our mothers, sisters, daughters and friends who have affected our lives in many ways. Survivors continue their paths and work touching our lives everyday, reminding us that our fight is needed and is just because there is a price to fight for. Reminding us that until the cure happens, there is no stone that should remain unturned, no places we should not go, no politician we should not talk to, no genes,proteins, and other molecules that could make a difference we should not explore, poke and tease. We could wander to other matters of our lives, but this month of October, we should renew our commitment to the fight for the cure of breast cancer.
Efforts made so far have made a meaningful difference, our eyes have opened to new dimensions of cancer research, and the belief in the cure has hardened because through advances in targeting therapy and genetic works, THE CURE IS MORE POSSIBLE, REACHABLE AND REAL!
All we need is cast off the doubt, stop infighting, keep the eyes open, and bring the cure to the shores of our daily reality! We have the means, we have the science, we are full of justified hope, let's keep on marching until the victory rings, making the CURE REAL, PALPABLE AND ALIVE!
A blog about research, awareness, prevention, treatment and survivorship of Breast Cancer and all cancers, including targeted scientific research and a grassroots approach to increase screening for cancer, especially in the low income and under-insured population of El Paso, Texas, with a view to expand this new health care model to many other 'minority' populations across the United States and beyond
Showing posts with label target therapy. Show all posts
Showing posts with label target therapy. Show all posts
Monday, October 7, 2013
Tuesday, April 2, 2013
MSR1, ASCC1, and CTHRC1 (Nomenclature of Genes in Esophageal cancer)
CTHRC1" is a protein that has the ability to inhibit collagen matrix synthesis.
Expression of Cthrc1 is increased in fibroblasts and chondrocytic cells in response to TGF-beta family members including BMP4, BMP2 and TGF-beta. Cthrc1 is also upregulated during tumorigenesis and metastasis;
CTHRC1 has been linked to major signaling pathways such as Wnt and TGF-beta. The ability of CTHRC1 to inhibit TGF-beta signaling via a reduction in Smad 2/Smad 3 (is to be noted!)
Location 8q22.3. (Leclair at al )
Once again this comment suggests that stimulation of growth factor induced secondarily by NF-kB /c-JUn amplification leads to secondary amplification which in this case happens to this gene. This gene comes into play in vascular remodeling suggesting invasiveness of the cancer. This is the stuff used by neurone to find their way down their passage. If it is expressed it marks cellular invasiveness. Please pay marked attention to the pathway with witch it is identified, a pathway we believe is very important but neglected. The Wnt pathway. This is the metastasis pathways, it correlates with metastatic disease and is the stuff you find in triple negative Breast cancer!
Suppression of Smad2 could prevent cancer induced by Irritations? and may be secondary cancers?
2.ASCC1.
This gene encodes a subunit of the activating signal cointegrator 1 (ASC-1) complex. The ASC-1 complex is a transcriptional coactivator that plays an important role in gene transactivation by multiple transcription factors including activating protein 1 (AP-1), nuclear factor kappa-B (NF-kB) and serum response factor (SRF). The encoded protein contains an N-terminal KH-type RNA-binding motif which is required for AP-1 transactivation by the ASC-1 complex. Mutations in this gene are associated with Barrett esophagus and esophageal adenocarcinoma. Alternatively spliced transcripts encoding multiple isoforms have been observed for this gene. [provided by RefSeq, Dec 2011]"" (danielsen et al!)
Activating signal cointegrator 1 complex subunit 1 (ASCC1) is a subunit of the activating signal cointegrator 1 (ASC-1) complex. The ASC-1 complex is a transcriptional coactivator that plays an important role in gene transactivation by multiple transcription factors including activating protein 1 (AP-1), nuclear factor kappa-B (NF-kB) and serum response factor (SRF). ASCC1 contains an N-terminal KH-type RNA-binding motif which is required for AP-1 transactivation by the ASC-1 complex. Mutations in the ASCC1 gene are associated with Barrett esophagus and esophageal adenocarcinoma [taken from NCBI Entrez Gene (Gene ID: 51008)].
MSR1
already discussed
Expression of Cthrc1 is increased in fibroblasts and chondrocytic cells in response to TGF-beta family members including BMP4, BMP2 and TGF-beta. Cthrc1 is also upregulated during tumorigenesis and metastasis;
CTHRC1 has been linked to major signaling pathways such as Wnt and TGF-beta. The ability of CTHRC1 to inhibit TGF-beta signaling via a reduction in Smad 2/Smad 3 (is to be noted!)
Location 8q22.3. (Leclair at al )
Once again this comment suggests that stimulation of growth factor induced secondarily by NF-kB /c-JUn amplification leads to secondary amplification which in this case happens to this gene. This gene comes into play in vascular remodeling suggesting invasiveness of the cancer. This is the stuff used by neurone to find their way down their passage. If it is expressed it marks cellular invasiveness. Please pay marked attention to the pathway with witch it is identified, a pathway we believe is very important but neglected. The Wnt pathway. This is the metastasis pathways, it correlates with metastatic disease and is the stuff you find in triple negative Breast cancer!
Suppression of Smad2 could prevent cancer induced by Irritations? and may be secondary cancers?
2.ASCC1.
This gene encodes a subunit of the activating signal cointegrator 1 (ASC-1) complex. The ASC-1 complex is a transcriptional coactivator that plays an important role in gene transactivation by multiple transcription factors including activating protein 1 (AP-1), nuclear factor kappa-B (NF-kB) and serum response factor (SRF). The encoded protein contains an N-terminal KH-type RNA-binding motif which is required for AP-1 transactivation by the ASC-1 complex. Mutations in this gene are associated with Barrett esophagus and esophageal adenocarcinoma. Alternatively spliced transcripts encoding multiple isoforms have been observed for this gene. [provided by RefSeq, Dec 2011]"" (danielsen et al!)
Activating signal cointegrator 1 complex subunit 1 (ASCC1) is a subunit of the activating signal cointegrator 1 (ASC-1) complex. The ASC-1 complex is a transcriptional coactivator that plays an important role in gene transactivation by multiple transcription factors including activating protein 1 (AP-1), nuclear factor kappa-B (NF-kB) and serum response factor (SRF). ASCC1 contains an N-terminal KH-type RNA-binding motif which is required for AP-1 transactivation by the ASC-1 complex. Mutations in the ASCC1 gene are associated with Barrett esophagus and esophageal adenocarcinoma [taken from NCBI Entrez Gene (Gene ID: 51008)].
Alternative names for ASCC1 Antibody include activating signal cointegrator 1 complex subunit 1 antibody, ASC-1 complex subunit p50 antibody, Trip4 complex subunit p50 antibody, p50 antibody, CGI-18 antibody, ASC1p50 antibody.
I refuse to comment on this one because it is so obvious, this is at the core of pathogenesis where chronic stimuli act through the NF-kB and C-JUN to induce growth factors which eventually stimulate a secondary amplification that leads to the pathogenesis of cancer, additional mutations such as that occurring in CTHRC1 will complete the dance. This ASCC1 appears to be a CBF like molecular complex driving this transformation and therefore it is a valid target for therapy.MSR1
already discussed
Sunday, March 24, 2013
GENES HYPERMETHYLATED TO FAVOR DEDIFFERENTIATION, AND NEOPLASTIC TRANSFORMATION IN LUNG CANCERS
RESEARCHERS SUGGEST THE FOLLOWING GENE AS TARGET FOR HYPERMETHYLATION: 1. DAPK
Death-associated protein kinase 1 is an enzyme that in humans is encoded by the DAPK1 gene.[1]
Death-associated protein kinase 1 is a positive mediator of gamma-interferon induced programmed cell death. DAPK1 encodes a structurally unique 160-kD calmodulin dependent serine-threonine kinase that carries 8 ankyrin repeats and 2 putative P-loop consensus sites. It is a tumor suppressor candidate.[2]
In melanocytic cells DAPK1 gene expression may be regulated by MITF.[3]"
AND YOU KNOW THAT ANYONE WHO WANTS TO LIVE WILL SILENCE THIS GENE. KILLING INTERFERON EFFECT IN LUNG CANCER DESPITE STRESS INDUCTION ROLE IN THE PATHOGENESIS OF LUNG CANCERS.
-------------------------------------------------------------------THIS GENE WAS DISCUSSED IN OTHER BLOG NOTE---------
2. GSTP1
Glutathione S-transferase P is an enzyme that in humans is encoded by the GSTP1 gene.[1][2]
Glutathione S-transferases (GSTs) are a family of enzymes that play an important role in detoxification by catalyzing the conjugation of many hydrophobic and electrophilic compounds with reduced glutathione. Based on their biochemical, immunologic, and structural properties, the soluble GSTs are categorized into 4 main classes: alpha, mu, pi, and theta. The glutathione S-transferase pi gene (GSTP1) is a polymorphic gene encoding active, functionally different GSTP1 variant proteins that are thought to function in xenobiotic metabolism and play a role in susceptibility to cancer, and other diseases.[3]
GSTP1 has been shown to interact with Fanconi anemia, complementation group C[4][5] and MAPK8.[6]"
METHYLATION HERE IS TO PERPETUATE THE ACTION OF CAUSING FACTORS. IT IS BAD FOR PATIENTS TO CONTINUE SMOKING ON TREATMENT. THIS IS AN EARLY EVENT IN TUMOR NEOPLASIA TRANSFORMATION.
EXPLAINING WHY RETINIOIC ACID (PREVENTION) AND ATRA MAY NOT WORK FULLY!
4.ECAD
5.p14 ARF
6.p16
7.TIMP1
8.FHIT
DAPK1
From Wikipedia, the free encyclopedia
Jump to: navigation, search
| Death-associated protein kinase 1 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
 PDB rendering based on 1ig1. |
|||||||||||
|
|||||||||||
| Identifiers | |||||||||||
| Symbols | DAPK1; DAPK | ||||||||||
| External IDs | OMIM: 600831 MGI: 1916885 HomoloGene: 3626 ChEMBL: 2558 GeneCards: DAPK1 Gene | ||||||||||
| EC number | 2.7.11.1 | ||||||||||
|
|||||||||||
| RNA expression pattern | |||||||||||
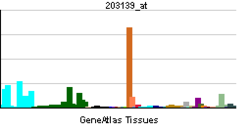 |
|||||||||||
 |
|||||||||||
| More reference expression data | |||||||||||
| Orthologs | |||||||||||
| Species | Human | Mouse | |||||||||
| Entrez | 1612 | 69635 | |||||||||
| Ensembl | ENSG00000196730 | ENSMUSG00000021559 | |||||||||
| UniProt | P53355 | Q80YE7 | |||||||||
| RefSeq (mRNA) | NM_004938 | NM_029653 | |||||||||
| RefSeq (protein) | NP_004929 | NP_083929 | |||||||||
| Location (UCSC) | Chr 9: 90.11 – 90.32 Mb |
Chr 13: 60.6 – 60.76 Mb |
|||||||||
| PubMed search | [1] | [2] | |||||||||
Death-associated protein kinase 1 is a positive mediator of gamma-interferon induced programmed cell death. DAPK1 encodes a structurally unique 160-kD calmodulin dependent serine-threonine kinase that carries 8 ankyrin repeats and 2 putative P-loop consensus sites. It is a tumor suppressor candidate.[2]
In melanocytic cells DAPK1 gene expression may be regulated by MITF.[3]"
AND YOU KNOW THAT ANYONE WHO WANTS TO LIVE WILL SILENCE THIS GENE. KILLING INTERFERON EFFECT IN LUNG CANCER DESPITE STRESS INDUCTION ROLE IN THE PATHOGENESIS OF LUNG CANCERS.
-------------------------------------------------------------------THIS GENE WAS DISCUSSED IN OTHER BLOG NOTE---------
2. GSTP1
GSTP1
From Wikipedia, the free encyclopedia
Jump to: navigation, search
| Glutathione S-transferase pi 1 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
 PDB rendering based on 10gs. |
|||||||||||
|
|||||||||||
| Identifiers | |||||||||||
| Symbols | GSTP1; DFN7; FAEES3; GST3; GSTP; PI | ||||||||||
| External IDs | OMIM: 134660 MGI: 95864 HomoloGene: 660 ChEMBL: 3902 GeneCards: GSTP1 Gene | ||||||||||
| EC number | 2.5.1.18 | ||||||||||
|
|||||||||||
| RNA expression pattern | |||||||||||
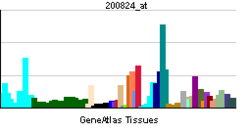 |
|||||||||||
| More reference expression data | |||||||||||
| Orthologs | |||||||||||
| Species | Human | Mouse | |||||||||
| Entrez | 2950 | 14869 | |||||||||
| Ensembl | ENSG00000084207 | ENSMUSG00000038155 | |||||||||
| UniProt | P09211 | P46425 | |||||||||
| RefSeq (mRNA) | NM_000852 | NM_181796 | |||||||||
| RefSeq (protein) | NP_000843 | NP_861461 | |||||||||
| Location (UCSC) | Chr 11: 67.35 – 67.35 Mb |
Chr 19: 4.04 – 4.04 Mb |
|||||||||
| PubMed search | [1] | [2] | |||||||||
Glutathione S-transferases (GSTs) are a family of enzymes that play an important role in detoxification by catalyzing the conjugation of many hydrophobic and electrophilic compounds with reduced glutathione. Based on their biochemical, immunologic, and structural properties, the soluble GSTs are categorized into 4 main classes: alpha, mu, pi, and theta. The glutathione S-transferase pi gene (GSTP1) is a polymorphic gene encoding active, functionally different GSTP1 variant proteins that are thought to function in xenobiotic metabolism and play a role in susceptibility to cancer, and other diseases.[3]
GSTP1 has been shown to interact with Fanconi anemia, complementation group C[4][5] and MAPK8.[6]"
METHYLATION HERE IS TO PERPETUATE THE ACTION OF CAUSING FACTORS. IT IS BAD FOR PATIENTS TO CONTINUE SMOKING ON TREATMENT. THIS IS AN EARLY EVENT IN TUMOR NEOPLASIA TRANSFORMATION.
Cyclic AMP mediated GSTP1 gene activation in tumor cells involves the interaction of activated CREB-1 with the GSTP1 CRE: a novel mechanism of cellular GSTP1 gene regulation.
PUTING THE EFFECT DEEP INTO THE MITOCHNDRIA. WHERE THE MTOR INHIBITORS WORK?
-------------------------------------------------------------------------------------------------
| 3.RAR BETA:This gene encodes retinoic acid receptor beta, a member
of the thyroid-steroid hormone receptor superfamily of nuclear |
4.ECAD
5.p14 ARF
6.p16
7.TIMP1
8.FHIT
Sunday, March 10, 2013
(CONFERENCE CONTINUES) PANCREATIC CANCER UPDATE:
*FOLFIRINOX definitely in control as first choice for first line
but this option is too toxic in the elderly so a modified version is adopted by some
.*new IMPACT STUDY, GEMZAR-ABRAXANE is being rapidly adopted as an alternative to FOLFIRINOX for this same and very reason (Toxicity of Folfirinox)
This combination was reportedly tried in selected clinics (including Eastern Europe) in a Phase III trial, was tried against Gemzar alone
and gave Progression free survival of 5.5 months Vs 3.7 months
Overall survival 8.5 months Vs 6.7 months (Von Hoff DD et al.)
Abraxane given at 125 mg/m2 and Gemzar at 1000mg/m2 Q3/4 in the combination arm
----------------------------------------------------------------------------------------------
3rd choice of course was GEMZAR-ERLOTINIB follwed by GEMZAR ALONE.
===========================================================
NOTABLY NO TARGET THERAPY DISCUSSED WHICH NEEDS TO BE CORRECTED FAST!
but this option is too toxic in the elderly so a modified version is adopted by some
.*new IMPACT STUDY, GEMZAR-ABRAXANE is being rapidly adopted as an alternative to FOLFIRINOX for this same and very reason (Toxicity of Folfirinox)
This combination was reportedly tried in selected clinics (including Eastern Europe) in a Phase III trial, was tried against Gemzar alone
and gave Progression free survival of 5.5 months Vs 3.7 months
Overall survival 8.5 months Vs 6.7 months (Von Hoff DD et al.)
Abraxane given at 125 mg/m2 and Gemzar at 1000mg/m2 Q3/4 in the combination arm
----------------------------------------------------------------------------------------------
3rd choice of course was GEMZAR-ERLOTINIB follwed by GEMZAR ALONE.
===========================================================
NOTABLY NO TARGET THERAPY DISCUSSED WHICH NEEDS TO BE CORRECTED FAST!
Wednesday, January 9, 2013
FOR THE CURE, TIME FOR PARADIGM SHIFT AND A REVOLUTION AGAINST SOME OF OUR LEADERS IN CANCER MEDICINE
Cancer is a disease involving the cell. Our current understanding is that during the course of our lives, somewhere in our system, a cell's function will be altered enough to transform a normal cell into A CANCER CELL. Our current understanding is that all cells want to stay alive and for cancer cell multiplication and dissemination it appears to be assurance of a type of cell preservation. We know that to survive, the cancer cell will escape several mechanisms. How to stimulate its growth, how to escape detection by the immune system and removal by the Macrophages and related natural measures, how to stay awake by lighting up certain pathways, how to resist against external chemical attacks, how to repair damages caused by attacks, how to survive on their own etc.?
We also know that cancer cells are not the same not only by tissue of origin, but also by pathways driving them. We know that to escape death, the cancer cell uses redundancies and loopholes in its pathways, that is it may alter or multiply these pathways to overrun incoming inhibitions. It may amplify measures to block our reach toward programmed death. The cancer cell knows that once programmed death mechanisms are started, it has to die. It builds things like Bcl-2 around the Caspase death path. The cancer cell knows that there are inhibitory forces that need to be altered. P53 is one of the Major forces. It needs to be altered or mutated. Flow through a pathway is another force. And altering regulators may be one way to control the flow. Or leaving a switch on to drive the pathways. etc...
We also know that every major target in pathways has effects downstream toward the nucleus and its DNA, and upstream toward the Membrane. For some, we have found lateral connections serving as loophole escape. More than one phenotype of an important Target is meant to provide Resistance to attacks of the main type.
With chemotherapy, we have had some success. Our failures reside in the mechanisms of resistance, in the ability of the cancer cell to repair itself and escape death. Escaping death appears to be also solely linked to protection against Necrosis and programmed death.
We also know about Driver pathways as well as forces we can use to stop cell migration, division and seeding. We have got to use this knowledge to plan our action for the cure.
The success of target therapy needs to tell us that leaders who continue to push chemotherapy as the only alternative, creating more combinations, need to be more and more left alone, while we switch to Targeting therapy and some combination therapies.
Targeting therapy tells us we got to get better at defining Driver pathways to be effective. Particularly in solid tumors. This is the major priority. HOW DO YOU TELL THIS IS A DRIVER TARGET OR PATHWAY? IS IT BY DOSING REGULATORY MOLECULES, ENZYMES ALONG A PATHWAY, LEVEL OF TRANSCRIPTION GENES, STATUS OF SWITCH TO TARGET MOLECULES, PROMOTER EXPRESSION? HOW DO YOU SAY THIS IS THE DRIVER PATHWAY? WITH THIS KNOWLEDGE WE CAN AVOID STUDIES LIKE TAXOTERE & REVLIMID IN PROSTATE CANCER, WHEN TAXOTERE & VELCADE WOULD HAVE BEEN BETTER.
IF WE KNOW HOW TO DO THIS, OUR PATH TO CURE IS ASSURED.
The second question: HOW TO GET THIS CELL TO CASPASE, TO LYSOZOMAL HYDROLASES AND CATHEPSINS, AND OTHER NECROTIC AND AUTOPHAGIC PROCESSES? HOW TO PUSH IT TO PROGRAMMED DEATH?
TIME TO WAKE UP AND SMELL THE COFFEE BEFORE ANOTHER RUN FOR THE CURE!
We also know that cancer cells are not the same not only by tissue of origin, but also by pathways driving them. We know that to escape death, the cancer cell uses redundancies and loopholes in its pathways, that is it may alter or multiply these pathways to overrun incoming inhibitions. It may amplify measures to block our reach toward programmed death. The cancer cell knows that once programmed death mechanisms are started, it has to die. It builds things like Bcl-2 around the Caspase death path. The cancer cell knows that there are inhibitory forces that need to be altered. P53 is one of the Major forces. It needs to be altered or mutated. Flow through a pathway is another force. And altering regulators may be one way to control the flow. Or leaving a switch on to drive the pathways. etc...
We also know that every major target in pathways has effects downstream toward the nucleus and its DNA, and upstream toward the Membrane. For some, we have found lateral connections serving as loophole escape. More than one phenotype of an important Target is meant to provide Resistance to attacks of the main type.
With chemotherapy, we have had some success. Our failures reside in the mechanisms of resistance, in the ability of the cancer cell to repair itself and escape death. Escaping death appears to be also solely linked to protection against Necrosis and programmed death.
We also know about Driver pathways as well as forces we can use to stop cell migration, division and seeding. We have got to use this knowledge to plan our action for the cure.
The success of target therapy needs to tell us that leaders who continue to push chemotherapy as the only alternative, creating more combinations, need to be more and more left alone, while we switch to Targeting therapy and some combination therapies.
Targeting therapy tells us we got to get better at defining Driver pathways to be effective. Particularly in solid tumors. This is the major priority. HOW DO YOU TELL THIS IS A DRIVER TARGET OR PATHWAY? IS IT BY DOSING REGULATORY MOLECULES, ENZYMES ALONG A PATHWAY, LEVEL OF TRANSCRIPTION GENES, STATUS OF SWITCH TO TARGET MOLECULES, PROMOTER EXPRESSION? HOW DO YOU SAY THIS IS THE DRIVER PATHWAY? WITH THIS KNOWLEDGE WE CAN AVOID STUDIES LIKE TAXOTERE & REVLIMID IN PROSTATE CANCER, WHEN TAXOTERE & VELCADE WOULD HAVE BEEN BETTER.
IF WE KNOW HOW TO DO THIS, OUR PATH TO CURE IS ASSURED.
The second question: HOW TO GET THIS CELL TO CASPASE, TO LYSOZOMAL HYDROLASES AND CATHEPSINS, AND OTHER NECROTIC AND AUTOPHAGIC PROCESSES? HOW TO PUSH IT TO PROGRAMMED DEATH?
TIME TO WAKE UP AND SMELL THE COFFEE BEFORE ANOTHER RUN FOR THE CURE!
Labels:
apoptosis,
cancer cell,
caspase,
cathepsins,
cell preservation,
crbcm,
dna,
enzymes,
lysozomal hydrolases,
macrophage,
nucleus,
pathway drivers,
target therapy,
taxotere,
velcade
Friday, November 2, 2012
The secret for Cure of cancer is located in the selective apoptosis, or cancer cell death
We know there are several ways that lead to cell death. The main 2 ways are through the Extrinsic pathway which uses Receptors located at the skin of the cell called cellular membrane (receptors such as TNF-R1 and FAS) and Intrinsic pathways that use internal proteins (i.e. Caspases) that may destroy or paralyze the breathing and energy producing organs of the cell called mitochondria. The challenge is to control these processes in the cell, know how to trigger them, and to do this only in the cancer cells without affecting the normal cells. We need to know how to tag cancer cells, give that tag to a killing molecule that can attach to the apoptosis receptor. This is just one way to be looking for a cure. The complexity and multitude of metabolic pathways presents a problem, but also opportunities to kill the cancer cell.We are in the wee hours of learning them.Target therapy is in its early hour.
When there is a mistake in the gene during replication, there is a repair mechanism. To allow that repair,
the cell needs to be slowed down in its life cycle. This slowing seems to be the main action of P53. If repair does not occur, P53 leads the cell to cell destruction/apoptosis. That's why most cancers remove or change the P53 to stay alive. Like most Molecules in the cell, the P53 has its own path to destruction. MDM2 seems to be that path to the loss of this so important P53. Scientists are looking at knocking down MDM2 to see if this may restore the P53 function in those conditions where the P53 is not fundamentally altered. We will follow this for you and give an update!
The Cure is achievable we know that for sure, we need just need to become better "cell mechanics"....stay tuned...
When there is a mistake in the gene during replication, there is a repair mechanism. To allow that repair,
the cell needs to be slowed down in its life cycle. This slowing seems to be the main action of P53. If repair does not occur, P53 leads the cell to cell destruction/apoptosis. That's why most cancers remove or change the P53 to stay alive. Like most Molecules in the cell, the P53 has its own path to destruction. MDM2 seems to be that path to the loss of this so important P53. Scientists are looking at knocking down MDM2 to see if this may restore the P53 function in those conditions where the P53 is not fundamentally altered. We will follow this for you and give an update!
The Cure is achievable we know that for sure, we need just need to become better "cell mechanics"....stay tuned...
Saturday, October 27, 2012
Building an Electronic Cancer Cell is a necessity
Natural death of cancer cells is the path to cure.
Experience of chemotherapy has shown that a blind and random attack of cancer cells is ineffective at assuring the death of cancer at a 100% curative rate. We believe that this is mostly due to the fact that chemotherapy most of the time does not inflict enough damage to the cell to lead to self destruction or Apoptosis. We believe that certain changes to the cell caused by chemotherapy could work counter the intended effect. This the basis of the trust in target therapy.
Now let us not approach Target therapy the same way we did for chemotherapy. Target therapy has proven to work, no doubt about it. We need now to organize coordinated attacks on the cancer cells. We know that Cancer cells' life processes seem to be organized in cascade, redundancy and escape mechanisms, but in a logical way. With one event following another. This is why Target therapy works by cutting off or promoting upstream events in the cascade.The thing is that cells have downstream escape mechanisms, therefore that mechanism needs also to be struck down in a staged or coordinated attack.
We believe that the construction of an electronic model of a cell will help us identify gaps in the cascade of molecular events, and help identify critical new targets to go after, once these gaps are filled.
Some of the current targets
1. Adhesion Molecules
2. Cell membrane receptors
3. Signal transduction pathways
4. Transcription genes
5. Histones and promoter genes
6. Mitochondrial/ribosomes Metabolism disruption
7. Nuclear genetic material
8. Gene repair and mismatch repair mechanism
This list is not exhaustive, therefore the potential for investigation appears endless.
Experience of chemotherapy has shown that a blind and random attack of cancer cells is ineffective at assuring the death of cancer at a 100% curative rate. We believe that this is mostly due to the fact that chemotherapy most of the time does not inflict enough damage to the cell to lead to self destruction or Apoptosis. We believe that certain changes to the cell caused by chemotherapy could work counter the intended effect. This the basis of the trust in target therapy.
Now let us not approach Target therapy the same way we did for chemotherapy. Target therapy has proven to work, no doubt about it. We need now to organize coordinated attacks on the cancer cells. We know that Cancer cells' life processes seem to be organized in cascade, redundancy and escape mechanisms, but in a logical way. With one event following another. This is why Target therapy works by cutting off or promoting upstream events in the cascade.The thing is that cells have downstream escape mechanisms, therefore that mechanism needs also to be struck down in a staged or coordinated attack.
We believe that the construction of an electronic model of a cell will help us identify gaps in the cascade of molecular events, and help identify critical new targets to go after, once these gaps are filled.
Some of the current targets
1. Adhesion Molecules
2. Cell membrane receptors
3. Signal transduction pathways
4. Transcription genes
5. Histones and promoter genes
6. Mitochondrial/ribosomes Metabolism disruption
7. Nuclear genetic material
8. Gene repair and mismatch repair mechanism
This list is not exhaustive, therefore the potential for investigation appears endless.
Tuesday, October 23, 2012
We believe in the cure for Cancer:
People talk about a cure and skeptics balk!
But the cure is possible and actually exists already in every survivor who had a remote history of cancer.
Remember this, a cancer cell is full of messages encrypted in chemical messages when to grow, when to start aging and when to die. Yes cancer cells have an internal message when to start apoptosis (self destruction).
It means you could tell it to start apoptosis and kill itself. Our challenge is to know how to speak to a cell.
Research are starting to learn that language in what is now known as Target Therapy. Cancer treatment is now becoming a Piano tune. if you hit the right keys in a song and the cancer cell get it, it will find its way to self destruction. We are at the early stage of this music, still learning it. Hitting this key here and seeing what happens. We are finding out that even tough cancers such as Melanoma, if you hit the BRAF key, things start happening. In some lung cancers, if you hit the EGFR key, you start getting somewhere. It is just a matter of time before we start asking to a cell, now time for an increase in BAX or Caspases, and self destruct. The cell has some redundancy and networking to complicate the road to self destruction, but we still believe that with the right tune, cancer cells will dance to self destruction, and yes cure is within our reach!
But the cure is possible and actually exists already in every survivor who had a remote history of cancer.
Remember this, a cancer cell is full of messages encrypted in chemical messages when to grow, when to start aging and when to die. Yes cancer cells have an internal message when to start apoptosis (self destruction).
It means you could tell it to start apoptosis and kill itself. Our challenge is to know how to speak to a cell.
Research are starting to learn that language in what is now known as Target Therapy. Cancer treatment is now becoming a Piano tune. if you hit the right keys in a song and the cancer cell get it, it will find its way to self destruction. We are at the early stage of this music, still learning it. Hitting this key here and seeing what happens. We are finding out that even tough cancers such as Melanoma, if you hit the BRAF key, things start happening. In some lung cancers, if you hit the EGFR key, you start getting somewhere. It is just a matter of time before we start asking to a cell, now time for an increase in BAX or Caspases, and self destruct. The cell has some redundancy and networking to complicate the road to self destruction, but we still believe that with the right tune, cancer cells will dance to self destruction, and yes cure is within our reach!
Sunday, October 21, 2012
Clinical Hypothesis in research, prevention and Commercialization Hypothesis in cancer therapeutics
Following our first article of October 14th, we believe it is time to suggest a second hypothesis
in therapeutic research in Cancer. The early years of cancer treatment, the objective was to blast the cancer cells with chemotherapy that was in our arsenal. Most of the time this approach was able to kill the cells partially. The cancer cells quickly however learned to escape the blast, creating wonderful resistance mechanisms. As we progress in molecular biology, we are increasingly shying away from these blast approaches, leaning more and more in identifying metabolic pathways, and identifying targets in that pathway and aiming our gun and shoot it, and see what happens. This is called Target Therapy.
One pathway that we have learned a bit about is the P53 ( and down the line the pathway the Rb which lead to cell stopping in the cell cycle to allow genetic repair). This pathway is mostly triggered by an abnormality in the gene.
Today, we go back to the blast approach when we have no good Target therapy option. In fact we always try to add the target therapy to the blast chemotherapy to see if we could have the most from our money.
combination of Avastin (a target therapy) to chemotherapy is standard therapy in the United states for stage IV Colon cancer. We know that chemotherapy mostly affect our gene. This change in gene should trigger the activation of our P53 system to stop the cancer cell in its track for growth. The question now is should we give chemotherapy in patient who has an altered P53 system. What is the benefit the gene with chemotherapy, if the system that should be triggered to clean up is out.
Hypothesis:
Altered P53 pathway predict a failure of chemotherapy which has gene disturbance as main effect.
second hypothesis: preservation of status of the wild type P53 during chemotherapy may predict for a successful chemotherapy treatment (Cisplatin).
if it is true, commercialization is possible...
Don't be shy, give me your opinion!
in therapeutic research in Cancer. The early years of cancer treatment, the objective was to blast the cancer cells with chemotherapy that was in our arsenal. Most of the time this approach was able to kill the cells partially. The cancer cells quickly however learned to escape the blast, creating wonderful resistance mechanisms. As we progress in molecular biology, we are increasingly shying away from these blast approaches, leaning more and more in identifying metabolic pathways, and identifying targets in that pathway and aiming our gun and shoot it, and see what happens. This is called Target Therapy.
One pathway that we have learned a bit about is the P53 ( and down the line the pathway the Rb which lead to cell stopping in the cell cycle to allow genetic repair). This pathway is mostly triggered by an abnormality in the gene.
Today, we go back to the blast approach when we have no good Target therapy option. In fact we always try to add the target therapy to the blast chemotherapy to see if we could have the most from our money.
combination of Avastin (a target therapy) to chemotherapy is standard therapy in the United states for stage IV Colon cancer. We know that chemotherapy mostly affect our gene. This change in gene should trigger the activation of our P53 system to stop the cancer cell in its track for growth. The question now is should we give chemotherapy in patient who has an altered P53 system. What is the benefit the gene with chemotherapy, if the system that should be triggered to clean up is out.
Hypothesis:
Altered P53 pathway predict a failure of chemotherapy which has gene disturbance as main effect.
second hypothesis: preservation of status of the wild type P53 during chemotherapy may predict for a successful chemotherapy treatment (Cisplatin).
if it is true, commercialization is possible...
Don't be shy, give me your opinion!
Subscribe to:
Comments (Atom)