 Patients With Macular Degeneration at Increased Death Risk
Patients With Macular Degeneration at Increased Death Risk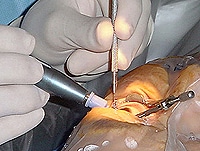 Cataract Surgeons See Laser's Potential in a New Light
Cataract Surgeons See Laser's Potential in a New Light FDA Approves Trulign Intraocular Lens
FDA Approves Trulign Intraocular Lens AREDS2: Insights Into Optimal Supplements for AMD
AREDS2: Insights Into Optimal Supplements for AMD
Glucosamine Linked to Increased Intraocular Pressure
Drug & Reference Information
Glucosamine supplementation was linked to
significant, reversible increases in intraocular pressure (IOP) in a
small, retrospective study published online May 23 in JAMA Ophthalmology.
However, the investigators, led by Ryan K. Murphy, DO, from the
University of New England College of Osteopathic Medicine, Biddeford,
Maine, and colleagues, could not exclude the potential for permanent
damage.
"Frequently, patients are being told that while studies give conflicting data as to whether glucosamine and chondroitin sulfate are effective in reducing arthritic pain, there does not appear to be any risk in trying these supplements," Andrew L. Sherman, MD, professor and vice chair of clinical rehabilitation medicine at the University of Miami Leonard M. Miller School of Medicine in Florida, told Medscape Medical News when asked for comment on the study. "This study, if [the findings are confirmed], attacks that premise."
US prevalence of osteoarthritis is 27 million, and for open-angle glaucoma, it exceeds 2 million, according to the Centers for Disease Control and Prevention.
"Although it is [unclear] what the implications of having increased IOP would be for individual patients, the risk is...that ocular damage could possibly occur from what were previously thought to be 'benign' supplements," said Dr. Sherman, who was not involved in the study.
A keen observation by coauthor Edward Hall Jaccoma, MD, clinical associate professor of ophthalmology at the University of New England College of Osteopathic Medicine, provided the impetus for this study.
"A family member I was following as a glaucoma suspect suddenly had a sharp rise in...IOP, and the only change in his life was adding glucosamine supplements for arthritis," Dr. Jaccoma told Medscape Medical News. "I made a tentative connection based on the molecular biology and potential kinship to steroid glaucoma. When he stopped the supplement, his IOP returned to baseline levels. Subsequent observations of...patients on these supplements appear to show an interaction similar to what [happened] in this index patient."
Study Design and Findings
The investigators retrospectively studied 6 men and 11 women, with a mean age of 76 years, who had a history of glucosamine supplementation and ocular hypertension (IOP > 21 mm Hg) or diagnosed open-angle glaucoma, a willingness to discontinue glucosamine, 3 or more IOP measurements within 2 years, and no associated changes in glaucoma medications or eye surgery. Group A (n = 11) had 1 to 3 baseline IOP measurements before starting glucosamine, and group B (n = 6) had no baseline IOP measurements.
IOP increased in group A after starting glucosamine supplementation (P = .001). After glucosamine discontinuation, IOP decreased in group A (P = .002), group B (P = .008), and groups A and B combined (19.5 ± 0.4 to 16.7 ± 3.0 mm Hg in the right eye and 20.3 ± 2.9 to 17.3 ± 2.4 mm Hg in the left eye; P < .001). For any categories or comparisons, the left and right eyes in each patient did not differ significantly.
"Many questions are raised by glucosamine supplementation–associated IOP changes," the study authors write. "This study shows a reversible effect of those changes, which is reassuring. However, the possibility that permanent damage can result from prolonged use of glucosamine supplementation is not eliminated."
Study Limitations and Implications
"Glucosamine supplements are a billion dollar business, and as the baby boom generation looks for ways to stave off their arthritis, more and more of them [turn] to what has been billed as a 'safe supplement,' " said Dr. Jaccoma, who is also director of Southern Maine Eye Associates in Sanford and of New England Dry Eye Center in Kennebunk, Maine. "My concern is that some...of them may end up with glaucomatous damage that could have been prevented or...medicating (or having laser and other surgical interventions) for a disease...that might have been avoided in the subset of 'glucosamine responders.' "
Dr. Jaccoma recommends that at the very least, people at risk for glaucoma have their IOP more closely monitored during glucosamine supplementation.
"I do have a small subset of patients who find glucosamine so helpful to their arthritis that they would prefer to treat the IOP [rather than] give up the supplements," he said. "The large [National Institutes of Health] study on glucosamine suggested there could be a group of arthritic patients who do benefit from this supplement, but the majority did not show much, if any, benefit. Given that data, it appears that many may be taking this supplement needlessly, if not dangerously."
Study limitations noted by the investigators and Dr. Sherman include its retrospective design and the very small sample with limited generalizability because it consisted of patients who were at least glaucoma suspects. The study did not account for glucosamine dosage, duration, brand, or compliance.
"[M]y personal observations suggest that the response is very similar to what we see with steroids, in that the average patient will have little IOP effect..., but that there is a higher risk group who must be identified to avoid harm from their steroid treatment," Dr. Jaccoma said. "I believe...we will find a similar...group that reacts this way to glucosamine..., but more research is needed."
Coauthor Mona Doss, MA, also from the University of New England
College of Osteopathic Medicine, suggests larger, randomized clinical
trials are needed to assess dose-dependent increase in IOP with
glucosamine supplementation in different patient groups.
"At this point in time more research is required to definitively change current management," she said. "The clinical implications may indicate consideration by primary care or other providers in recommending such supplementation for arthritis in patients with known risk of elevated IOP or glaucoma."
"These results will need to be replicated in a larger population of patients to be felt to be entirely reliable," Dr. Sherman concluded. "{After confirming] these results with a larger study, [they should] study the real clinical implications of this increase in IOP for...those with and without glaucoma."
The study authors and Dr. Sherman have disclosed no relevant financial relationships.
JAMA Ophthalmol. Published online May 23, 2013. Extract
"Frequently, patients are being told that while studies give conflicting data as to whether glucosamine and chondroitin sulfate are effective in reducing arthritic pain, there does not appear to be any risk in trying these supplements," Andrew L. Sherman, MD, professor and vice chair of clinical rehabilitation medicine at the University of Miami Leonard M. Miller School of Medicine in Florida, told Medscape Medical News when asked for comment on the study. "This study, if [the findings are confirmed], attacks that premise."
US prevalence of osteoarthritis is 27 million, and for open-angle glaucoma, it exceeds 2 million, according to the Centers for Disease Control and Prevention.
"Although it is [unclear] what the implications of having increased IOP would be for individual patients, the risk is...that ocular damage could possibly occur from what were previously thought to be 'benign' supplements," said Dr. Sherman, who was not involved in the study.
A keen observation by coauthor Edward Hall Jaccoma, MD, clinical associate professor of ophthalmology at the University of New England College of Osteopathic Medicine, provided the impetus for this study.
"A family member I was following as a glaucoma suspect suddenly had a sharp rise in...IOP, and the only change in his life was adding glucosamine supplements for arthritis," Dr. Jaccoma told Medscape Medical News. "I made a tentative connection based on the molecular biology and potential kinship to steroid glaucoma. When he stopped the supplement, his IOP returned to baseline levels. Subsequent observations of...patients on these supplements appear to show an interaction similar to what [happened] in this index patient."
Study Design and Findings
The investigators retrospectively studied 6 men and 11 women, with a mean age of 76 years, who had a history of glucosamine supplementation and ocular hypertension (IOP > 21 mm Hg) or diagnosed open-angle glaucoma, a willingness to discontinue glucosamine, 3 or more IOP measurements within 2 years, and no associated changes in glaucoma medications or eye surgery. Group A (n = 11) had 1 to 3 baseline IOP measurements before starting glucosamine, and group B (n = 6) had no baseline IOP measurements.
IOP increased in group A after starting glucosamine supplementation (P = .001). After glucosamine discontinuation, IOP decreased in group A (P = .002), group B (P = .008), and groups A and B combined (19.5 ± 0.4 to 16.7 ± 3.0 mm Hg in the right eye and 20.3 ± 2.9 to 17.3 ± 2.4 mm Hg in the left eye; P < .001). For any categories or comparisons, the left and right eyes in each patient did not differ significantly.
"Many questions are raised by glucosamine supplementation–associated IOP changes," the study authors write. "This study shows a reversible effect of those changes, which is reassuring. However, the possibility that permanent damage can result from prolonged use of glucosamine supplementation is not eliminated."
Study Limitations and Implications
"Glucosamine supplements are a billion dollar business, and as the baby boom generation looks for ways to stave off their arthritis, more and more of them [turn] to what has been billed as a 'safe supplement,' " said Dr. Jaccoma, who is also director of Southern Maine Eye Associates in Sanford and of New England Dry Eye Center in Kennebunk, Maine. "My concern is that some...of them may end up with glaucomatous damage that could have been prevented or...medicating (or having laser and other surgical interventions) for a disease...that might have been avoided in the subset of 'glucosamine responders.' "
Dr. Jaccoma recommends that at the very least, people at risk for glaucoma have their IOP more closely monitored during glucosamine supplementation.
"I do have a small subset of patients who find glucosamine so helpful to their arthritis that they would prefer to treat the IOP [rather than] give up the supplements," he said. "The large [National Institutes of Health] study on glucosamine suggested there could be a group of arthritic patients who do benefit from this supplement, but the majority did not show much, if any, benefit. Given that data, it appears that many may be taking this supplement needlessly, if not dangerously."
Study limitations noted by the investigators and Dr. Sherman include its retrospective design and the very small sample with limited generalizability because it consisted of patients who were at least glaucoma suspects. The study did not account for glucosamine dosage, duration, brand, or compliance.
"[M]y personal observations suggest that the response is very similar to what we see with steroids, in that the average patient will have little IOP effect..., but that there is a higher risk group who must be identified to avoid harm from their steroid treatment," Dr. Jaccoma said. "I believe...we will find a similar...group that reacts this way to glucosamine..., but more research is needed."
Medical-Billing.com
can help you manage your revenue cycle to improve collections and get
paid faster and without denials—all for less than the cost of in-house
billing.
Information from Industry
"At this point in time more research is required to definitively change current management," she said. "The clinical implications may indicate consideration by primary care or other providers in recommending such supplementation for arthritis in patients with known risk of elevated IOP or glaucoma."
"These results will need to be replicated in a larger population of patients to be felt to be entirely reliable," Dr. Sherman concluded. "{After confirming] these results with a larger study, [they should] study the real clinical implications of this increase in IOP for...those with and without glaucoma."
The study authors and Dr. Sherman have disclosed no relevant financial relationships.
JAMA Ophthalmol. Published online May 23, 2013. Extract

No comments:
Post a Comment